1) Welcome to a new #accredited #tweetorial on currently available treatments for mineralocorticoid receptor (MR) antagonism (#MRA), the differences among them, and how these differences impact on treatment of cardio-reno-metabolic diseases #CaReMe #FOAMed
2) Our expert author is Dr. Patrick Holmes MB BS, MSc, DipTher, MRCGP (@drpatrickholmes), a GP Partner at St. George’s Medical Practice, Darlington for 23 years. He is a Trustee for the Primary Care Diabetes Society and is Associate Editor for Diabetic Medicine @DiabeticMed.

3) This program is supported by an educational grant from Bayer & is intended for #healthcare providers. Author disclosures can be found at http://ckd-ce.com/disclosures/. Prior programs, still available for CE/#CME credit, are at http://ckd-ce.com. CE/#CME credit 🇬🇧🇪🇺🇨🇦🇺🇸
4) Credit available for #physicians #physicianassociates #nurses #nursepractioners #pharmacists First, a poll. Which of the following are potential unwanted effects of MR antagonism using spironolactone? Answer before you scroll ⤵️!
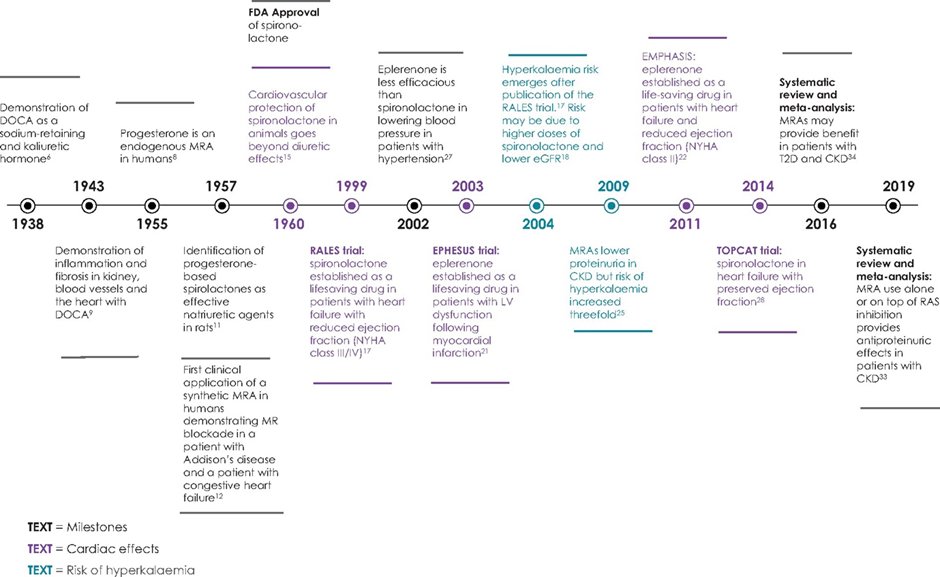
5) The answer is d, hypokalaemia. Spironolactone is associated w/⬆️risk of #hyperkalaemia. Before investigating the differences in the currently commercially available #MRAs, let's review the basics. MR is a steroid hormone receptor.
6) Steroid hormone receptors [e.g., androgen receptor, progesterone receptor, glucocorticoid receptor (GR) etc…] are a sub-family of intracellular receptors & nuclear transcription factors.
7) The MR has a complex structure, with a DNA-binding domain that interacts with the nuclear DNA, a ligand-binding domain as well as two areas of activation function.
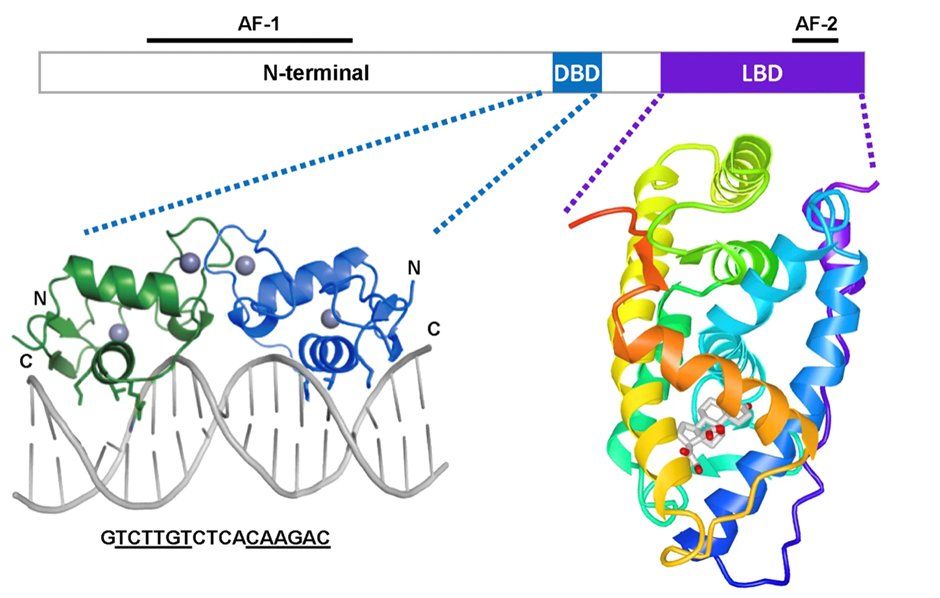
8) Whilst the GR is activated by the hormone/ligand cortisol, the MR is promiscuous with the same binding affinity for aldosterone & cortisol. Furthermore, progesterone competes with aldosterone for MR binding with similar affinity, acting as a MRA. (https://onlinelibrary.wiley.com/doi/10.1002/cphy.c130044)
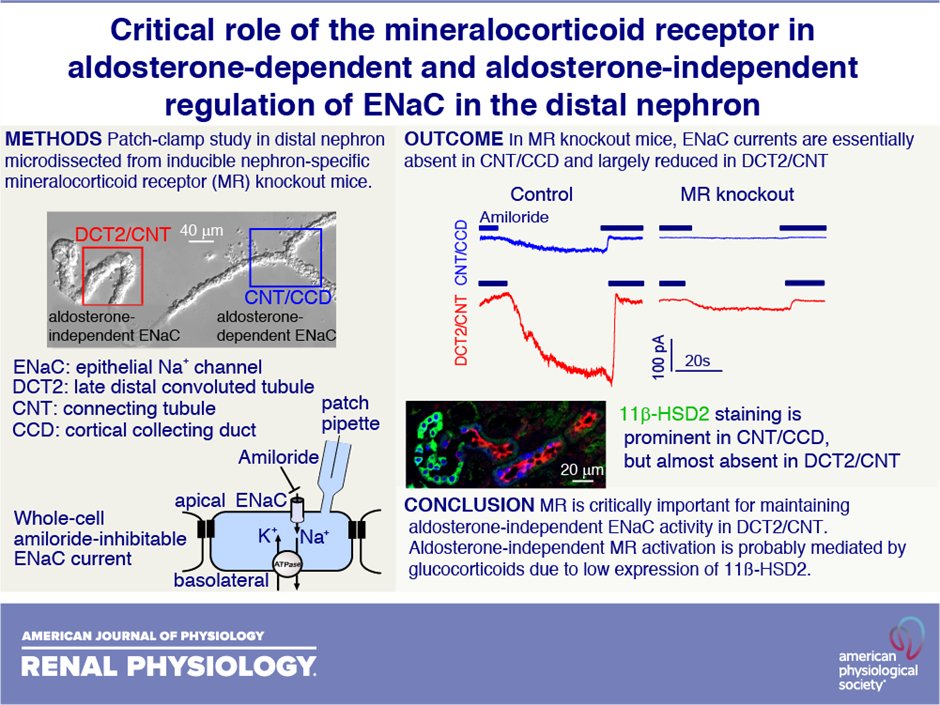
9) In 1987 the MR gene was cloned. This in turn led to animal experiments using MR knock-out (MRKO) strains compared to normal ‘wild-type’ strain animals. Typically, rodents.
10) Complete MRKO is lethal with 10 days of birth due to the ensuing severe pseudohyperaldosteronism, thus demonstrating the critical importance of MR in salt, water, & #bloodpressure maintenance during early life.
11) MRKO cardiac cells compared to wild-type in a myocardial infarction 🐭 model led to :
⤴️ infarct healing
👉improved cardiac remodelling
⤵️ pulmonary oedema
⤵️ contractile dysfunction
12) Myeloid MRKO gives us insights into the key role of MR and inflammation and fibrosis. In a glomerulonephritis model, podocyte MRKO provided no kidney protection.
13) However myeloid MKRO led to
⤵️ proteinuria
⤵️ cardiac hypertrophy
⤵️ fibrosis
⤵️ inflammation
⤵️ endothelial sodium channel circuits
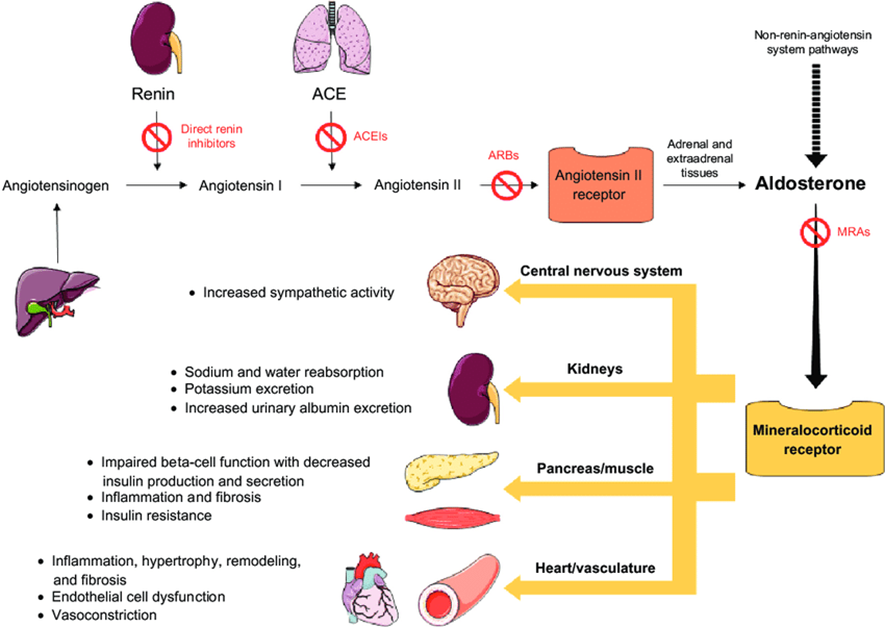
14) This leads to aldosterone driving physiological MR activity in those tissues, whereas in the cardiomyocytes cortisol is also a major active MR ligand. Long-term use of ACEi/ARBs use in #heartfailure, #CKD or #hypertension can lead to “aldosterone breakthrough’ …
15) … due to incomplete suppression of serum aldosterone levels that may also worsen MR overstimulation.
https://www.nature.com/articles/ncpneph0575
The image below summarises the downstream effects of MR activation
🔓
16) Next up: comparisons of the commercially available MRA’s. MRA’s differ significantly in chemical structure, which in term drives significant differences in their clinical utility. 1st & 2nd generation MRAs are steroidal, and not dissimilar to aldosterone.
17) 3rd generation MRA’s are non-steroidal and belong to the dihydropyridine chemical class.
👉1st generation MRAs = #spironolactone & #canrenone
👉2nd generation MRA = #eplerenone
👉3rd generation MRA = #finerenone & #esaxerenone
18) Return tomorrow for more education from @GoggleDocs principal @drpatrickholmes and your link to grab 0.5h CE/#CME on options for #MRA! Nods to @drkevinfernando @HannahBeba @AmarPut @edgarvlermamd @ChristosArgyrop @sophia_kidney @nephondemand @dguerrot @goKDIGO
19a) Welcome back! You're differentiating among mineralocorticoid receptor antagonists #MRAs with expert faculty @drpatrickholmes. Follow this thread to your CE/#CME! Tip my hat to @parthaskar @kamleshkhunti @DiabetesUK @drpratikc @docwas @AliRacaniere @DSNforumUK @profmjdavies
19b) & profuse apologies from the vast @ckd_ce home office for the posting error in tweet 4. Many of you realized that we had left out the “NOT” in the❓, but the point is that steroidal #MRAs are assoc'd w/gynecomastia/mastodynia, impotence/⬇️libido, hypotension & HYPERkalemia.
20) For the rest of the tweetorial I have focused on the 2 most widely used steroidal MRAs (spironolactone & eplerenone) & the only 2 commercially available non-steroidal MRAs (finerenone & esaxerenone). Below is a summary of the key pharmacodynamic & pharmacokinetic data.
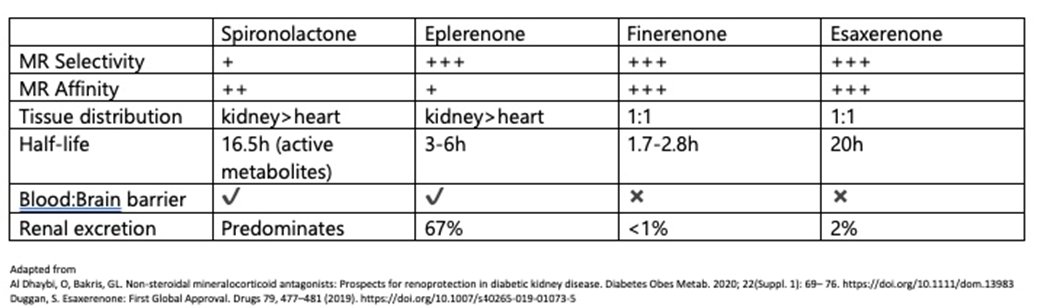
21) Re the importance of MR selectivity: spironolactone’s lack of selectivity for the MR, w/ binding to both progesterone & androgen receptors. leads to gynecomastia (10x⤴️in RALES).
Eplerenone, finerenone & esaxerenone in RCTs had similar rates of gynecomastia to placebo.
22) Renal tissue selectivity, high renal excretion, high MR affinity & long half-life all likely drive risk of hyperkalaemia (🔓https://academic.oup.com/eurheartj/article/42/2/152/5936792).
👉Hyperkalaemia rates spironolactone > eplerenone
👉Rates steroidal MRAs > non-steroidal MRAs
👉Risks⤴️ as kidney function⤵️
23) So what about impact on blood pressure ⁉️
Spironolactone is thought to ⤵️BP than other MRAs.(https://link.springer.com/article/10.1007%2Fs11906-019-0924-0)
Eplerenone ⤵️BP more than finerenone (🔓https://academic.oup.com/eurheartj/article/37/27/2105/1749451)
whereas eplerenone has a similar impact on BP as esaxerenone (🔓https://www.ahajournals.org/doi/full/10.1161/HYPERTENSIONAHA.119.13569)
24) Here at @ckd_ce we are keen to focus on the utility of MRAs in the treatment of #CKD. Due to the risk of hyperkalaemia, steroidal MRAs have a limited role in #CKD. Of the non-steroidal MRAs only finerenone is licensed for CKD in people with #type2diabetes (currently only 🇺🇸)

25) So let's leave you with a 3-part, rapid-fire knowledge check: first, which MRA has a 🇺🇸 license for the treatment of CKD in people with type 2 diabetes? Mark your answer before you scroll down!
26) The answer is c, #finerenone. 🇺🇸 approval for the treatment of adult patients with #CKD associated w/ #T2D was based on the results from the phase 3 FIDELIO-DKD trial (🔓https://www.nejm.org/doi/full/10.1056/NEJMoa2025845):
27) Second, what was the relative increased risk of hyperkalaemia with spironolactone in the RALES study compared to placebo?
28) In the RALES trial (🔓https://pubmed.ncbi.nlm.nih.gov/10471456/), hyperkalaemia was in fact seen🔟times more often in patients treated with spironolactone than with placebo, and serious hyperkaelemia occurred twice as often (choice d).
29) BTW, check out https://cardiometabolic-ce.com/category/hyperkalemia/ for several opportunities to learn and earn CE/#CME on contemporary management of hyperkalemia, including facilitation of #RAASi.
30) Finally, finerenone is associated with what risk of developing gynaecomastia compared to placebo in the combined analysis of the FIGARO & FIDELITY trials?
31) The answer is: (b), about the same risk, removing the potential for a compliance problem for ♂️s who use steroidal #MRAs. See 🔓https://link.springer.com/article/10.1186%2F1472-6904-11-4.
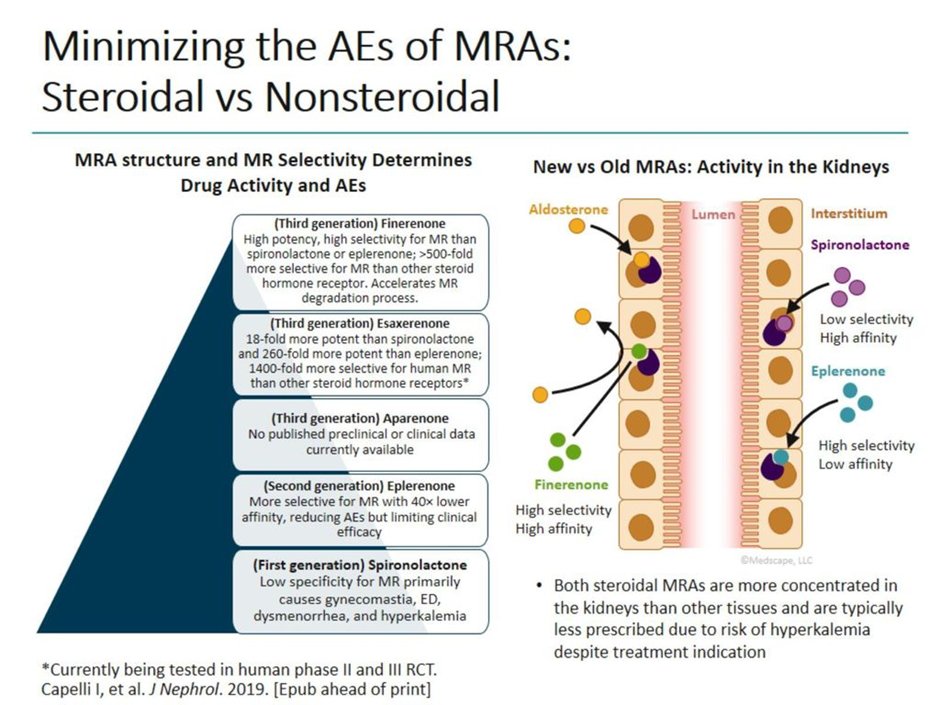
32) In summary, as per @AgarwalRajivMD, nonsteroidal MRAs appear to demonstrate a better benefit–risk ratio than steroidal MRAs, and given that overactivation of the MR leads to inflammation and fibrosis in cardiorenal disease, they represent an important advance!
33) And that's it–you have just earned 0.5h CE/#CME! Go to http://www.ckd-ce.com/MRA2 to claim your credit, and FOLLOW US for more education by #tweetorial, all FREE, all by EXPERT authors! I am @drpatrickholmes of @GoggleDocs. Be sure to follow @cardiomet_CE as well!
Originally tweeted by @CKD_ce (@ckd_ce) on February 15, 2022.
